Collagen is currently one of the most popular supplements. The promise: better cartilage, tendon and joint health, which would be important for every athlete, because it may reduce the likelihoodof injury and/or improve recovery after a connective tissue injury. Hence, it is worth taking a closer look at the mechanism and overall scientific evidence of its effectiveness on pain reduction and joint health.
Background
In 2019, it was estimated that 57 million people in Western Europe had osteoarthritis, a condition in which the articular cartilage wears away, exposing the underlying bone, oftentimes causing chronic pain and requiring surgical treatment (1). In athletes, connective tissue injuries are the most often reported type of injuries. It is therefore not surprising, that there is a big interest in finding strategies that may result in better soft tissue quality and/or support healing properties of cartilage, tendons and ligaments.
In this context, collagen is of major interest, as it provides structural support to the extracellular space of connective tissues. Collagen is the most abundant protein in connective tissue is collagen and specifically type I collagen. The strength and stiffness of our connective tissues and tendons is therefore determined in part by the amount of collagen they contain. It is therefore reasonable to assume, that improving collagen synthesis may indirectly lead to better joint and connective tissue quality and decrease risk of injuries (2).
In this article I will assess the evidence of collagen supplements on joint health
Collagen is a protein-based structure which is made of amino acids. In contrast to muscle tissue, it contains less essential amino acids and more Proline and Glycine.
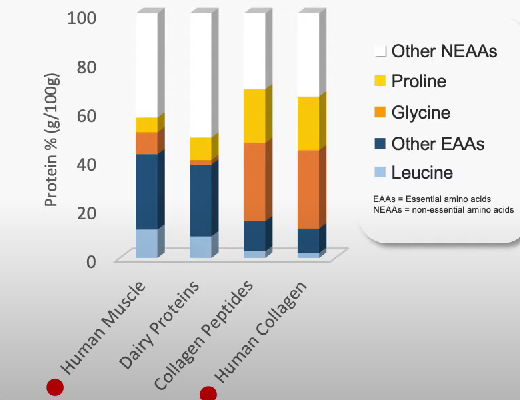
This leads to the hypothesis that the intake of certain nutrients, that contain high amounts of proline and glycine, could potentially have an anabolic stimuli on collagen synthesis rate, and thereby improve joint health of athletes and patients with arthritis. In this context two nutrients of interest are collagen-derived dietary-protein sources gelatine and collagen hydrolysate as they contain higher amounts of proline and glycine than other protein sources.
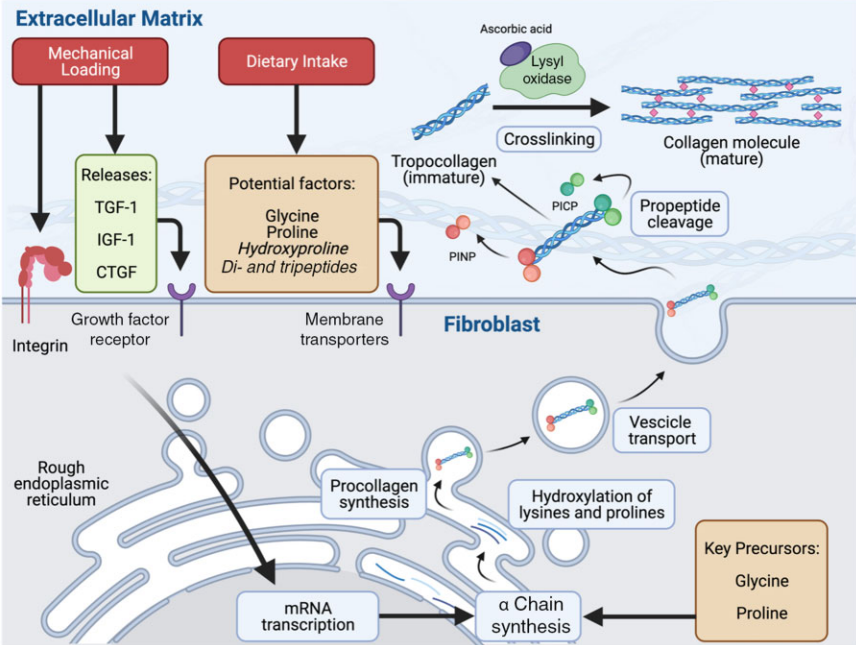
Collagen metabolism (3)
But aren’t gelatine and collagen of low protein quality?
It is true that gelatine and collagen possess rather low quality properties for a protein – at least if you use the biological value to assess protein quality. However, you need to consider what the biological value actually intends to do – and that is comparing the composition of protein rich foods to the amino acids matrix of human muscle (4). So yes, gelatine and collagen are not well-suited candidates to make you look jacked. In fact, recent studies have found no positive effect of collagen supplementation on muscle protein synthesis (5). However, this does not automatically mean they cannot have a positive impact on other tissue.
How well is gelatine digested and absorbed?
An early mechanistic study in 1999 found that gelatine hydrolysate is indeed absorbed by mice and results in an accumulation of gelatine hydrolysate in the cartilage tissue (6).
Nearly two decades later, researchers were able to verify these observations in humans (7). In a cross-over study design, eight healthy subjects consumed either 0, 5 or 15g of Gelatine enriched with 48 mg of Vitamin-C sixty minutes before completing 6 min of rope skipping.
The findings:
The intake of 15g of Vitamin-C enriched Gelatine resulted in a significant increase of glycine and proline concentration in the blood, which showcases that these “lower quality” proteins are indeed absorbed and result in a significant increase of the amino acids glycine and proline in the blood., which play a key role in the process of collagen synthesis.
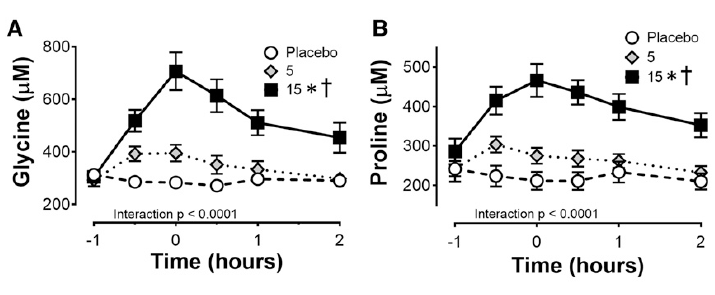
Glycine and proline concentrations in the blood after consuming 0, 5 or 15g of Gelatine – Vitamin-C enriched (7)
A significant positive effect on collagen syntheses rate (+ 153%) was measured via amino-terminal propeptide (PINP), which is a precursor of collagen and contains a short signal sequence and terminal extension peptides. The researcher were also able to detect an increased concentration of collagen in the engineered ligament.
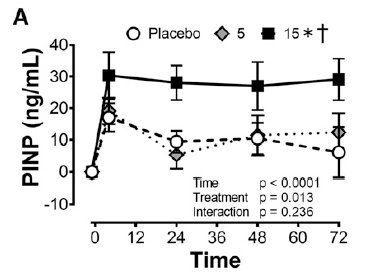
Collagen synthesis rate measured via PINP, with 0, 5 and 15g of Gelatine – Vitamin-C enriched (7)
What about collagen?
The same group of researcher did a follow-up study where they compared the effect of 15g of hydrolysed collagen vs. 15g gelatine (vitamin-c enriched) vs. gummi bears that contained both gelatine and collagen (8).
The results?
Both collagen supplementation, as well as gelatine (vitamin-c enriched), resulted in a ~ 20% increase in collagen synthesis rate. However, the change was not statistically significant. Moreover, if you look closer at the individual response of the participants, a large individual variance becomes apparent . By closer inspection of the individual data, it seems the overall positive effect is likely to be caused by one positive outlier – both in the gelatine and the collagen group. In fact, in 3 out of the 8 participants no positive change of the collagen synthesis rate was measured in the gelatine group, and 4 out of the 8 participant no effect was observed in the gelatine group.

Therefore, it is questionable whether these positive findings can be applied to the public
Moreover, it is worth mentioning that the researcher used again a manufactured a ligament in both their studies. In fact, up to this point we are lacking any human studies confirming these finding in humans.
Giving these two circumstances, I think we need more studies with larger cohorts verify these findings before we can say with certainty that gelatine/collagen supplementation does have a positive impact on collagen synthesis. There are, however, more studies we can look at to better assess the overall effect on joint and ligament health.
For example, McLindon and colleagues (9) investigated the effect of daily supplementation of 10g of collagen hydrolysate on mild knee osteoarthritis over a timespan of 48 weeks. The long duration of the study is definitely a big plus. The researchers also assessed cartilage function by taking dGEMRIC images, which is a much better indicator of changes in the cartilage tissue than measuring its acute synthesis rate over a short period (10, 11).
And indeed, a positive effect can clearly be seen when looking at the images below:
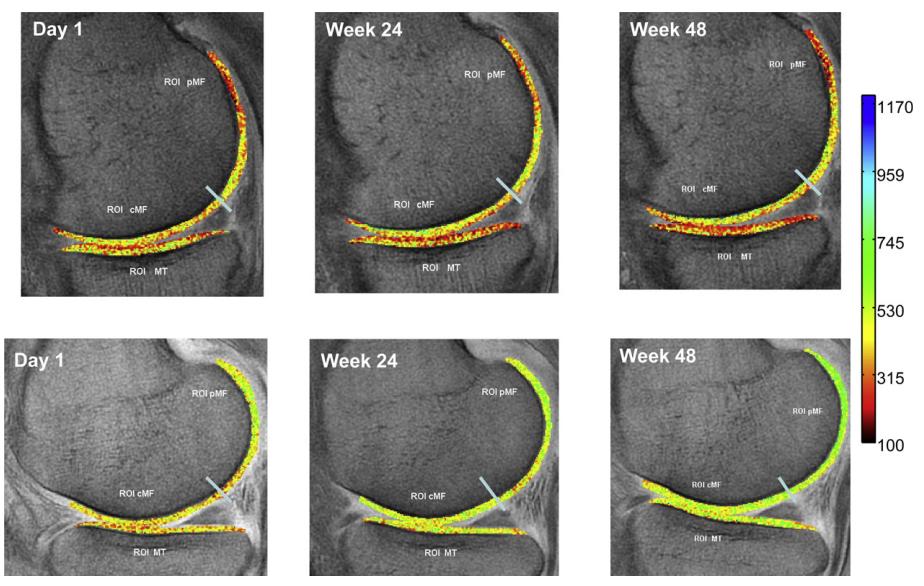
lower photo series is from collagen supplementation group and shows more green = better cartilage health
Does that prove that collagen supplementation is indeed effective for improving cartilage damage?
Not so fast!
The used dGEMRIC images showed improvements of cartilage in the posterior lateral femur region; with the collagen group having a statistical better improvement than the control group. However, further MRI images of cartilage tissue in other regions (medial tibia, central media femur, posterior medial femur, lateral tibia, central lateral femur) did not show any differences between the collagen and placebo group.
In fact, the author’s conclusion was:
In contrast to the dGEMRIC results, the T2 cartilage measures showed little variability or change with time, and no differences in any region between groups […] because of the pilot nature of this study, and its small sample size, we do not regard these results to be definitive, and the CH intervention merits further testing in a larger study.
It remains unclear, why the collagen group showed some improvement in certain areas and no change in others. With only 15 participants per group, the sample size of this study is too small to draw definite conclusions, and unfortunately there are no other studies available that used dGEMRIC images to assess changes in cartilage structure.
Effect of collagen on tendon and ligament stiffness & functionality
The same study from above (9) also assessed potential changes in physical functionality and stiffness, but failed to find a positive effect of collagen supplementation. It should be noted though that participants did not carry out a systematic training regimen to strengthen muscles, tendons or other soft tissue. This may be the explanation as to why McAlindon et al. 2011 (9) did not find a positive effect, because resistance exercise is a required stimulus for collagen synthesis (12).
In another study, Leet et al. (2003) did find a small benefit 30g of daily collagen hydrosylate supplementation (+ 500mg of vitamin-c) on patellar tendon stiffness in female football players [COL, +18.0 ± 12.2% (d = 1.11) vs. PLA, +5.1 ± 10.4% (d = 0.23), p = 0.049]. Albeit, tendon growth was similar between groups (13).
In another study 40 healthy young men trained their calve muscle and Achilles tendon for 14 weeks, 3 training sessions per week, and took 5g of collagen peptides (CP – Temdeforte®) (14). As far as I know, this is the only study where participants followed a structured resistance training protocol for more a 3 months period during which the training weight was progressively increased. Perhaps this is the reason the authors were able to detect a significantly (p = 0.002) greater increase in tendon growth (CSA +11.0%) compared to the PLA group (+4.7%). In contrast, there was no difference in tendon stiffness or muscle strength increased between groups.
Praes et al. (2019) used a similar supplementation protocol: in a double-blinded RCT with cross-over design 10 participants with Achilles Tendinopathy took 2.5g of CP for a duration of 6 months in combination with a bi-daily calf-strengthening programme (15). They also found no benefit of CP on tendon micro-vascularity assessed through contrast-enhanced ultrasonography (CEUS). CP supplementation also had no effect on ankle functionality and tendon pain evaluated through the VISA-A questionnaire (15).
The author did find a positive trend towards faster return to sport was observed in athletes who took CP. However, too few test subjects participated in the study to allow for a statistical analysis to be carried out. In other words: we don’t know whether the observed differences are due to chance or if they are truly the result of CP supplementation.
Interestingly, this study is often cited and used as a reference on how effective CP supplementation is, despite not showing any statistical significant effect.
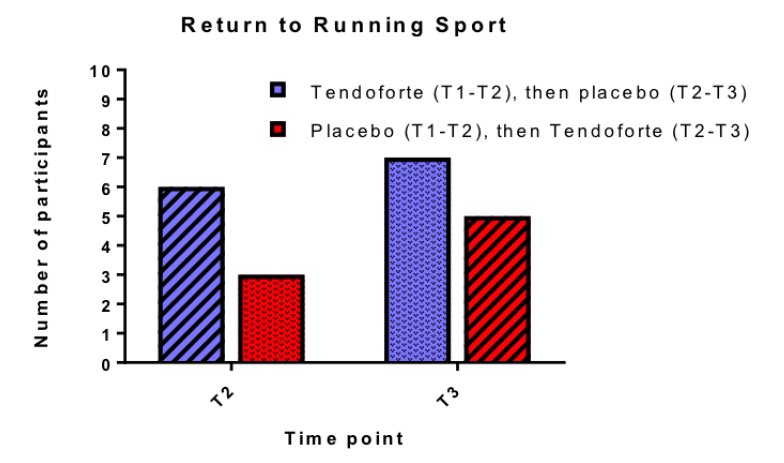
Praet et al., (2019): due to low number of participants, researchers did not carry out a chi-square t-test
Can it reduce pain?
Multiple studies suggest that there may be small benefit of collagen supplements on arthritis related pain (16,17,18). This improvement in pain sensation was measured both, subjectively from the patients as well as conformed by standardized tests by doctors.
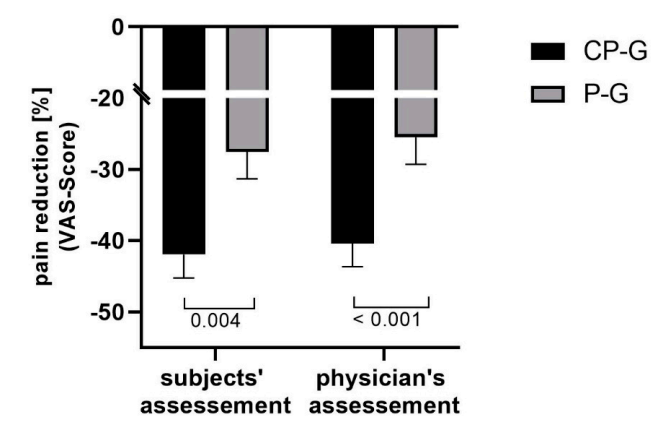
Relative changes in activity-related pain (VAS Score) (16)
However, it should be noted that other studies didn’t find a positive effect on pain reduction (19).
So what does that mean for using collagen as an anti-pain treatment?
From a practical standpoint, I would put collagen into the category of “it is worth trying”, if someone is really suffering from arthritis related pain. If you don’t notice a difference after ~8 weeks, just stop taking it. The overall effect will likely be small to moderate, as most studies report a reduction in pain sensation in the range of 15-20% in comparison to placebo.
Effectiveness of Whey and Casein
It seems natural to assume that high quality protein sources, such as Whey or Casein protein, are likely have a positive effect on collagen synthesis, considering protein sources with lower quality have been reported to
Surprisingly, this does not seem the case. Multiple studies using Whey protein did not find any positive affect on intramuscular connective tissue or collagen synthesis rate (20, 21).
One hypostasis as to why these studies failed to find an effect on connective tissue synthesis, is that Whey protein is basically metabolised “too fast” and that the activation of connective tissue is occuring delayed, and hence requires a slower absorbed protein to optimally be stimulated.
source: Nutrition Tactics
This hypothesis was investigated by Trommelen et al., (2020): While they did find that exercise itself activated connective tissue synthesis rate, there was no extra benefit observed when 30g of casein protein were consumed after resistance training (22).
Connective tissue proteins contain high concentrations of proline (12%) and glycine (25%) relative to other proteins within skeletal muscle. Casein on the other hand contains only small amounts of proline (6.5%) and glycine (2%) and may, therefore, provide insufficient amounts of these important amino acids to support postexercise increase in muscle connective tissue protein synthesis rate (23). This hypothesis is supported by the fact that the administered Casein by Trommelen et al. (2020) failed to elevate glycine concentrations in the blood.
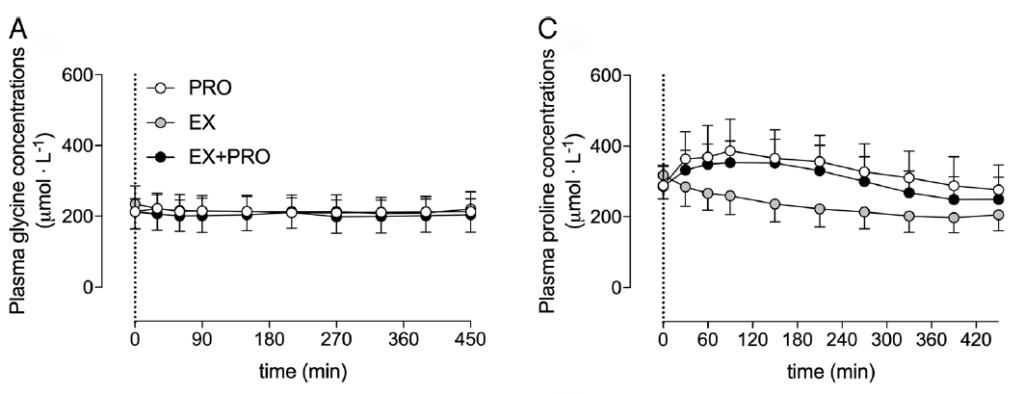
Changes in glycine and proline concentrations after consuming 30g of casein (Trommelen et al., 2020)
What if the amount of consumed protein would be increased?
This question was investigated by a follow-up study of the same researchers (24): In this study older men consumed 40g of casein after a bout of resistance exercise, and it was measured whether the consumption of the protein shake had an additional effect on connective tissue synthesis.
we demonstrate for the first time that dietary protein-derived amino acids are incorporated into de novo muscle connective tissue protein in older adults
The consumption of 40g of casein protein did indeed have a positive effect on connective tissue synthesis rate.
Summary:
- mechanistic in-vitro studies show that collagen and gelatine have a significant positive effect on cartilage synthesis rates
- in patients with chronic joint pain, continuous supplementation with collagen over 8 weeks or longer may reduce subjective pain levels by 15-20%
- weak evidence that collagen supplementation actually improves cartilage health
- weak to moderate evidence that collagen improves tendon stiffness
- it seems as both Whey and Casein protein do not have any significant effect on cartilage tissue, even if consumed in higher amounts
- we’re lacking high quality RCTs in humans to draw final conclusions about potential positive effects of collagen supplementation on joint and tendon health
My assessement
Overall evidence for improving joint health

The overall evidence is mixed; with some studies showing promising results. However, if you look at the details of those studies, almost all of them contain methodological weaknesses. The results from mechanistic studies, as well as the positive results with regards to pain reduction, are somewhat promising, but we need more high-quality RCT’s with humans to be able to draw a more distinct conclusion.
